First aid for people with Alzheimer's

Ahmed Raza
 Written by
Sarah Gehrke, MSN, RN,
Sarah has worked in various roles at Coffee Medical Center including nurse, education director, and quality assurance director.
Written by
Sarah Gehrke, MSN, RN,
Sarah has worked in various roles at Coffee Medical Center including nurse, education director, and quality assurance director.
More than 5 million Americans and 47 million people worldwide live with dementia. This number is expected to skyrocket along with the increase in the elderly population. Despite what many people believe, the majority of individuals with dementia live at home, not in assisted living or nursing homes.
- 2022 Alzheimer's disease facts and figures — a report on the latest facts and figures from the Alzheimer's Association.
Family, friends, and professional caregivers provide the needed care in the communities where you live, protect and serve. If you encounter an individual with dementia in your community, would you know how to modify your actions appropriately?
Here are tips to prepare you to recognize dementia and respond to situations efficiently.
Learn about Alzheimer’s disease
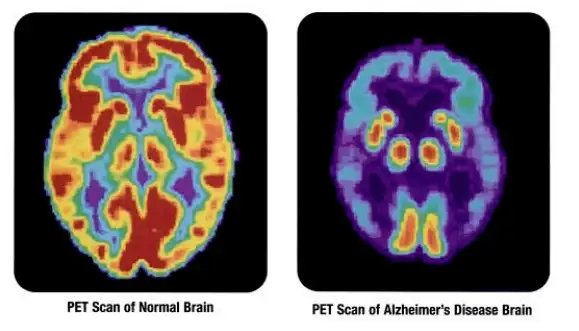
PET scans showing the differences between a normal older adult’s brain and the brain of an older adult who has Alzheimer’s disease. (User:7mike5000 / Creative Commons / CC0 1.0)
Learning about Alzheimer’s disease is the first step to ensure you know how to determine the best response to situations involving a person with dementia.
The term “dementia” comprises a group of conditions that cause a progressive deterioration in mental function, such as memory, behavior, logic, language, and movement. Dementia can make it difficult to manage day-to-day life, and as the disease progresses, a person will require more assistance from others.
Researchers are on the edge of understanding many aspects of these neurological conditions. No cure exists, but therapies are available that may help with symptoms and slow the rate of decline.
- Basics of Alzheimer's disease and dementia — learn about Alzheimer's disease and different types of dementia.
- Treatment of Alzheimer's disease — articles related to the current treatment approaches to Alzheimer's disease and other dementias.
Recognize Alzheimer’s disease
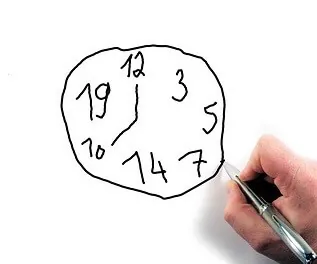
Clock-drawing test. (User: geralt / Creative Commons / CC0 1.0)
Providing first aid for people with Alzheimer’s can be a challenge, and it’s crucial to remember that no two people are the same. The following tips will help you identify someone with dementia. The person may:
- Appear disoriented and confused.
- Appear fearful, agitated, frustrated, angry, or is crying.
- Have a facial expression that is inappropriate in relation to the circumstances or have a flat affect.
- Have difficulty with gait and balance, which may be mistaken for intoxication.
- Reply with inappropriate answers or not respond at all.
- Not comprehend the situation or be unable to tell you their name, address, or where they are going.
- Not know the date, time or when they left their home.
- Have difficulty following directions.
- Dress inappropriately for the temperature.
- Be advanced in age (although, dementia can affect those under the age of 65).
Common situations
As a first responder or healthcare provider, you may encounter an individual with Alzheimer’s in various situations and conditions.
Here are some typical circumstances adapted from the Alzheimer’s Association’s first responder training program:
False accusations
An individual with Alzheimer’s may call the police station or emergency services to report a burglary, when in fact, the person has lost or misplaced the item.
Inappropriate behavior
Confusion, memory loss, and emotional reactions may produce improper actions, such as taking off their clothes in public. The person with dementia does not understand this is inappropriate behavior.
Shoplifting
Confusion and memory loss may cause a person to forget to pay for items in a store or even fail to recognize that it is required to pay for things before leaving the store.
Wandering or getting lost
People with Alzheimer’s can get lost easily at any time of the day. Assess for signs of dementia when encountering anyone that you suspect is wandering or lost.
After you recognize that someone may have dementia:
Look for a body-worn MedicAlert ID. If in the US, connect with MedicAlert + Alzheimer’s association safe return, a 24-hour nationwide emergency response service that provides access to:
- Caregiver contact information.
- Medical information.
- Assistance with found individuals who are not enrolled.
If the person is not enrolled, share this resource with the family or caregiver to encourage enrollment.
Fires
A person with dementia may leave the oven on or forget to turn off a burner. Also, it is not uncommon for the individual to mix up the seconds and minutes when using the microwave, thus burning the food in the microwave.
Hoarding
Poor judgment can cause a person to neglect themselves and their home, which can lead to safety risks and violation of fire codes. Hoarding may lead to fires, spoiled food, pests, and fall hazards.
Abuse and neglect
Situations of abuse and neglect can be stressful and require a thoughtful response.
- If an injury is noted, transport the person to a hospital immediately.
- If the person is in immediate danger, but not hurt, move the person to a safe location.
- If the individual is not in immediate danger, offer a referral to local resources.
- Always involve Adult Protective Services.
Firearms
When responding to a domestic call involving a person with dementia, ask the family or caregiver if there are weapons in the home. Firearms are in 60% of households where a person with dementia lives.
Judgment and personality changes can make having a weapon very dangerous for a person with dementia and others living in the home.
Leaving a firearm unloaded may not be enough. The person can still brandish a gun and cause an unsafe situation. Because of dementia, a person:
- May have extreme reactions to everyday events, such as mistaking a family member for a burglar.
- Can misinterpret surroundings and believe that something violent is happening in real-life when it is actually on TV.
- May overreact to surroundings and become overwhelmed by a doorbell or children playing.
If a family wishes to keep weapons in the home, they should:
- Store the firearms in a locked container or gun safe.
- Keep the key in a safe place.
- Store the unloaded firearm with a locking device.
Medical and disaster emergencies
During an evacuation, it is essential to keep the person with dementia calm. To do so:
- Avoid restraint or physical force.
- Be imaginative when communicating rather than rely on reality.
- Provide specific one-on-one guidance by using simple words.
- Attempt to relocate the person to a quiet place.
- Use distraction by giving the person a simple task.
- Ensure the person is observed at all times.
Communication strategies
The further the disease progresses, the less a person will be able to express or understand what is said.
Remember that communication can be both verbal and nonverbal. Your body language, tone, and volume of your voice can be just as important as your words.
The following communication strategies, which are adapted from Alzheimer’s Society of Canada’s First Responder Handbook and A Handbook for Care, may be helpful when approaching a person with dementia.
- Identify yourself and establish eye contact. Let the person know you are there to help.
- Speak slow and present one idea at a time.
- Establish a caring atmosphere. If you are approaching an individual who is upset or emotional, your composure may help to calm the individual. A sense of humor may help to defuse a stressful situation.
- Move the person to a quieter area to decrease distractions. Activity may make it difficult for a person with dementia to concentrate.
- Ask closed-ended questions that require simple answers, such as “yes” or “no.” “Do you know this street?” is easier to answer than “Where do you live?” Attempt to limit reality checks.
- Use actions to back up your words. If possible, demonstrate what you need the person to do by using non-verbal communication, such as point to the chair if you are asking the person to sit down. You may need to sit down next to them.
- Listen carefully to what the person is trying to say. You may not understand all of the spoken words, but you may recognize emotions, such as fear or anger. You can acknowledge the person's feelings by saying, "You seem upset."
- Watch for nonverbal signs. The person may not be able to express themselves adequately with words. Rubbing a body part may indicate pain. Tugging on or attempting to remove clothing may be a sign the person needs the restroom.
- Repeat and rephrase responses. If it is difficult to understand the person, try to repeat or rephrase what is said to ensure you understood correctly.
Additional resources
- First responder access and functional training series — video series designed to educate first responders on the various sensitivities related to those with Alzheimer's.
- Detect and prevent Alzheimer's disease before memory loss: TEDx Talk — Dr. Bernard Hanseeuw discusses that the hallmark pathologies of Alzheimer’s can be detected using a PET-scan many years before the onset of symptoms and what this means for future therapies.
- Gut microbiome alterations in Alzheimer's disease — an abstract that suggests that alterations in the gut microbiome may contribute to amyloid deposition.
- Towards understanding brain-gut-microbiome connections in Alzheimer's disease — a data-driven approach that shows how the human gut microbial metabolites may contribute to Alzheimer's.
- Neuroinflammation in the pathogenesis of Alzheimer's disease — new research avenues to prevent brain impairment based on nutritional supplements, dietary changes, and nutraceuticals.
- The healthy brain initiative — resources for the public health community to embrace a multifaceted approach to cognitive health.
- Map out a plan to approach Alzheimer's — a navigation tool that guides caregivers to information, local recourses, and support; this includes legal and financial planning.
- Alzheimer's Association home page — provides access to research, professionals, and valuable resources.
- ALZconnected — Alzheimer's Association's message board for caregivers.
- Banyan place — Take a look at the resources on this page if you or someone you know is considering assisted living, especially in Florida.
Do you have a first aid tip? Let us know! You can contact us at PMT support to reach the author.
Test your knowledge
- About 20 million people
- About 47 million people
- About 100 million people
- About 10 million people
- In nursing homes
- At home, not in assisted living or nursing homes
- In hospitals
- In assisted living facilities
- Only check for identification cards
- Look for a body-worn MedicAlert ID and connect with MedicAlert + Alzheimer's association safe return
- Immediately call the police
- Ask them complex questions to test their memory
- Accurate reports of actual crimes
- False accusations of burglary when they have actually lost or misplaced items
- Complaints about medical treatment
- Reports of family members stealing
- They are intentionally shoplifting
- Confusion and memory loss may cause them to forget to pay or fail to recognize that payment is required
- They are testing the store's security system
- They don't have enough money
Stay on track!
Would you like a reminder when your ACLS certification expires, plus study tips?
How we reviewed this article
Our experts continually monitor the medical science space, and we update our articles when new information becomes available.
-
Current versionMail the author of this page
- Oct 29, 2025
-
Copy edited by:
Copy editors - Mar 14, 2018
-
Reviewed by:
 Amanda Spier, RN, BSN Amanda Spier is a charge nurse in the emergency department of a regional hospital.
Amanda Spier, RN, BSN Amanda Spier is a charge nurse in the emergency department of a regional hospital. - Oct 21, 2017
-
Written by:
 Sarah Gehrke, MSN, RN Sarah has worked in various roles at Coffee Medical Center including nurse, education director, and quality assurance director.
Sarah Gehrke, MSN, RN Sarah has worked in various roles at Coffee Medical Center including nurse, education director, and quality assurance director.